Just three years ago, Patrisa Williams, who has chronic obstructive pulmonary disease (COPD), could not breathe without using her oxygen tank. Now, she’s hiking regularly with her grandchildren.
The dramatic improvement is thanks to a minimally invasive endobronchial valve placement she received at UC Davis Health – one of the first such procedures done in Northern California.
One of 16 million Americans diagnosed with COPD, Williams had difficulty breathing despite optimal medical therapy, pulmonary rehabilitation and even supplemental oxygen. COPD refers to a group of diseases that cause shortness of breath in part because areas within the lungs are diseased and holding trapped air (hyperinflation of the lung).
Williams has the emphysematous form of COPD. Patients with this type of COPD can have severe hyperinflation, leading to impairment of the muscles that drive breathing. This makes it difficult to inhale and fill the lungs with new air. COPD can limit a patient's ability to work or even do simple daily tasks.
“I needed to be attached to my portable oxygen tank 24/7,” recalled Williams. “I could not do anything without it. My blood oxygen levels would drop too low. I felt trapped and desperately wanted to find a way to have some sort of normalcy.”
Seeking treatment
To find a solution, Williams sought care with UC Davis Health. She met with Michael Schivo, co-director of the Comprehensive COPD Clinic, to optimize her care and to be evaluated for a procedure newly approved by the FDA to treat the emphysematous form of COPD. After a thorough discussion of her case at a UC Davis Interventional Therapeutics Board Committee meeting, she was referred to interventional pulmonologist Ken Yoneda for a final evaluation before her procedure.

Following her procedure, Patrisa Williams is now able to hike and spend quality time with her grandchildren.s
“At that time, we had recently concluded our participation in a large multi-centered clinical trial for endobronchial valve placement. It was the pivotal study that led the FDA to approve a minimally invasive procedure which places tiny valves in the airways allowing the healthier part of the lungs to expand,” Yoneda explained. “We are highly selective of the patients we choose for this procedure, but Patrisa met all our criteria.”
UC Davis Health is one of the few institutions in California performing endobronchial valve placement procedures. Patients who meet the minimum criteria for the procedure:
- Have a confirmed diagnosis of COPD with emphysema
- Have hyperinflated lungs
- Are not eligible for a lung transplant
Williams became the first patient treated with this procedure at UC Davis and one of the first in Northern California.
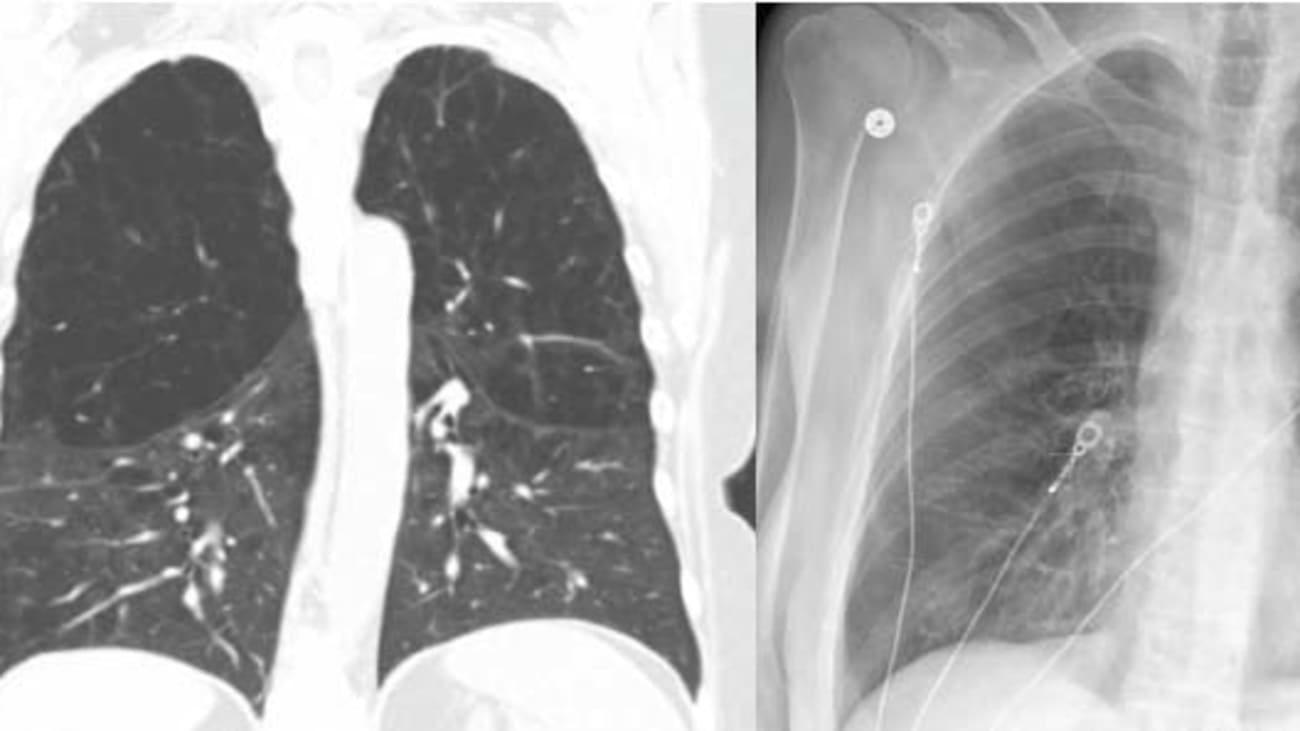
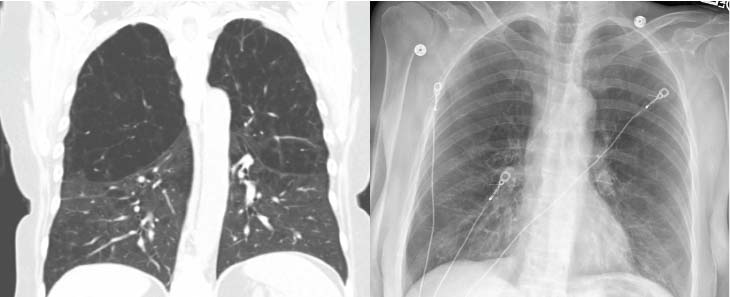
Endobronchial valve placement procedure
During the procedure, a standard bronchoscope and flexible delivery catheter are used to guide the valves into the target lobe and desired airway. Multiple valves are implanted to ensure complete occlusion of all airways leading to the target lobe of the lung. Valves may be placed at the lobar, segmental or subsegmental levels depending on the airway anatomy.
Once placed, the valve closes when the person inhales, keeping air out of the diseased area of the lung. It opens when the person exhales, allowing air to exit the lung and reducing the shortness of breath that occurs when the damaged part of the lung works hard to try to take in and push out air. By closing the diseased parts of the lungs off from the respiratory process, the endobronchial valve allows the healthier parts of the lungs to do their job better.
“For patients with limited respiratory function, the procedure provides improvements when inhaled medications and rehabilitation don’t,” Yoneda explained. “After treatment, the remaining lobes can now expand more fully and pressure on the diaphragm is relieved, improving their breathing mechanics and overall lung function. However, I can’t stress enough that patient selection and optimal COPD treatment are of paramount importance to the success of this procedure. Our COPD pulmonologists Brooks Kuhn and Michael Schivo are the cornerstone of that process.”
"For patients with limited respiratory function, the procedure provides improvements when inhaled medications and rehabilitation don’t.”
— Ken Yoneda
Improved quality of life
Following her procedure, Williams spent three nights recovering in the hospital. She spent much of her time resting in bed.
“The biggest risk for a patient following the procedure is a pneumothorax, so we monitor them closely and take a daily chest x-ray to make sure they are doing well,” Yoneda said. “We try to limit what they do, to stay in bed, and not cough for the first 24 hours. Then slowly, and over the next three days, we get them moving around.”
When Williams returned home, she restarted pulmonary rehabilitation and exercising. Just five months after the procedure, she began hiking and has not looked back.
"Since my procedure, I have not needed to use oxygen at all. I can breathe so much better. For me, it was a miracle. It has given me back the quality of life I was lacking.”
— Patrisa Williams
“Since my procedure, I have not needed to use oxygen at all,” Williams explained. “I can breathe so much better. For me, it was a miracle. It has given me back the quality of life I was lacking.”
Williams is grateful to everyone at UC Davis Health – from Yoneda, to the lung navigator who coordinated her care, to each nurse, technician and food service team member she encountered.
“Their entire team made it so easy for me. It was like they held my hand through the entire process,” she recalled. “Dr. Yoneda is the most caring doctor. He even called me when I got home to check on me. That personal touch made such a difference in the care I received.”
