Chapters
Transcript
RALPH J. DAMIANO: Thank you, Richard, and good evening. It's great to be here on this wonderful panel, and I would say it's a tremendous pleasure to work with my colleagues up here in the hypertrophic cardiomyopathy center. And I think it's been a great experience over the last 15 years of our group and the growth we've had at Wash U.
I'd like to talk to you about some new approaches to the surgical management of hypertrophic cardiomyopathy over the next 20 minutes. These are my disclosures. But particularly talk to you about some of the new minimally invasive surgical approaches that have been defined.
I would like to talk about-- which I think is an under-recognized problem in these patients-- is atrial fibrillation. And in my mind, that risk and the presence of atrial fibrillation is a real reason to consider septal myectomy in the appropriate patient over alcohol ablation. And also talk about some surgical approaches that have been brought forward to address. Residual mitral regurgitation, or mitral disease in patients with hypertrophic cardiomyopathy.
So let's start with minimally invasive septal myectomy. I think the indications for interventional treatment have been discussed in a prior talk by Richard, but clearly symptoms refractory to medical management and LV outflow tract obstruction greater than or equal to 50 millimeters of mercury at rest or with provocation, I think Richard went through that and that's been emphasized again in the most recent guidelines, which was in the European society. And the septal reduction therapy is really a class 1B indication in that situation.
But it's interesting in the European guidelines that a 1C indication is that patients that are referred for septal reduction therapy should be-- that that should be performed by experienced operators working as part of a multidisciplinary team expert in the management. And I think the decision of how to proceed is really a group decision, and that's how it should be approached where you do have expertise in all that and then make a decision on what's best for the individual patient.
It's interesting when you look at septal myectomy. It's one of the oldest operations in cardiac surgery, and as I like to tell my Fellows it's the most simple operation that's actually one of the most difficult to learn. It is very simple and it doesn't take a long time, but it has many pitfalls and it's much more of an art than a science.
Since that initial description back in the early 60s, really at the very birth of cardiac surgery, the operation has been modified in some minor ways but really remains essentially the same where we're removing that hypertrophied muscle from the outflow track. Initially, in the 70s, some surgeons were proposing to just do mitral valve replacement, but I think that has been rightfully abandoned in all Centers of Excellence. And really, in my opinion, has no role in the present management of this problem.
This is a picture from Leon Schlossberg from the Hopkins group that was really used in the original description that was done by Doctor Morrow, and you can see it's a pretty simple idea. You just retract the aortic valve of the right coronary cusp and remove a section of septum. You have to be careful where you remove that. That relieves the outflow tract obstruction.
There's some advantages to surgery that I think are worth talking about in that, since this is an operation that's been around for decades, we have very good evidence of long-term symptom relief and survival benefit when done at experienced centers. The other thing surgery-- and Richard mentioned that-- the other thing surgery allows you to do is to have direct visualization of the outflow tract anatomy and the associated mitral valve and papillary muscle abnormalities. In particular, sub-aortic membranes, which Richard showed you. In our experience, we do see at fairly regular intervals.
The other thing surgery allows is correction of associate cardiac lesions. I'm going to talk about atrial fibrillation, but also if there's associated mitral pathology or other outflow tract problems. Another nice thing about surgery, particularly in young patients as opposed to alcohol ablation, is you really don't have a postoperative myocardial infarction. And a much less scar burn, which has been shown.
And, at least both in our center and certainly in other centers with even larger experience, the operative mortality in the modern era is extremely low. And this is just a table taken from an article by Doctor Marin just looking at the consecutive myectomies without an operative death at some of the high-volume centers in North America. And you can see the Mayo Clinic. 800 without a death.
And really this is an operation, while some patients are somewhat hesitant to go ahead with, it's probably I would say the safest operation in modern cardiac surgery. This is our experience, and you can see in the darker line with just isolated septal myectomy that there's really not-- we've not had a mortality in the five-year experience-- clearly we have a smaller experience than at Mayo, but the five-year survival is excellent. Not so much in the patients who have concomitant procedures, and they often can be very complicated patients.
When we look at our late results in septal myectomy-- I'll just show you-- there really is excellent late results. We've had 176 patients with 4.5-year average follow up. The New York Heart Association class of follow-up, as Richard showed, after alcohol ablation is excellent at 89%. In the isolated myectomy group, it's 94%. And very few patients have residual mitral regurgitation, and it's very rare for that to be actually symptomatic.
Now, clearly there's some disadvantages to surgery and that is it does require an experienced team. Though I think that's an advantage if you're with that experienced team. But it is considered by patients to be quite invasive, and Richard illustrated that in this case study.
But there has been progress, and I wanted to just quickly review some of that, to make that surgery less invasive. And one of the approaches we've had in Saint Louis is to, instead of using a full sternotomy to go to a mini sternotomy approach, which leaves I think for patients-- you can see the scar right here. Particularly for women, a much more acceptable scar.
And this is just visualization of one of the cases. And basically, it's a small incision. You divide just the upper third of the sternum and the skin incision is between just the second and fourth intercostal spaces. But it allows for excellent visualization of the outflow tract. And just to orient the non-surgeons in the audience, this is the aorta right here. And up here-- you can do central cannulation. You can also do femoral venous calculation, but this is the venous cannula. This the aortic cannula. You can see with a small incision like this, really the only thing you do see is the aorta.
But you can see right here the excellent visualization where my forceps are of the outflow tract. And you can see the anterior leaf of the mitral valve. And it's a very excellent way in patients, particularly with other outflow tract anomalies. And I won't go through the details of myectomy, but if any of you are aspiring cardiac surgeons you can come to me afterwards.
We've had an experience we just recently presented, and it's in press with our experience with minimally invasive septal myectomy. And we compared 24 patients who had a full sternotomy to 49 patients who had a mini sternotomy. And this was prospectively study.
And just to summarize, it's a very safe operation so it's very hard to demonstrate any benefit from a minimally invasive approach, but we didn't see-- the good news is the two groups were comparable in terms of their preoperative demographics, but we really saw no difference in our interoperative results, particularly in terms of the time it took to do the operation. Aortic cross clamp and bypass times were exactly the same, and there was no difference in blood product usage. Albeit, this is a small, non-randomized trial.
In terms of post-operative complications, really we saw no mortality in either group and a very, very low rate of post-operative complications actually in these patients, and no significant differences between groups. There was also no significant differences in length of stay.
There's also been a group, mainly from Europe, describing an approach that's through the mitral valve. And the advantage for patients is you can then use a right mini thoracotomy, which is our approach of choice for isolated mitral valve disease. In this approach, you can go through-- it avoids the sternum completely, and you can actually work through the mitral valve. We generally do not use any rib spreading and just use a soft tissue retractor, which is like a large rubber band. And that prevents a lot of the post-operative pain than we traditionally saw and you can see-- just retract the anterior leaflet.
Some surgeons are now actually dividing the anterior leaflets, and it provides excellent view of the septum, though I would think this is really only indicated, in my opinion, in patients with associated mitral pathology because I really think that the results from a transaortic approach are excellent and this would unnecessarily complicate a routine patient. But those are the associated pathologies. This allows a minimally invasive approach and I think is an excellent option.
So these minimally invasive approaches are feasible. I think they have the potential, certainly, to further reduce surgical trauma. We'll need a lot more numbers to ever show that, but I think they also may help with patient acceptance, particularly in appropriate cases. And certainly, at least it's been our experience, that these minimally invasive incisions can achieve the same excellent results that have been reported with full sternotomy.
I'd like to switch gears now and just address atrial fibrillation in patients with hypertrophic cardiomyopathy, and it is a common sequelae. It's estimated that over the course of your lifetime you'll have about a 20% risk of developing AFib if you have hypertrophic cardiomyopathy and it may be as high as 40% in patients who live to 70 years or older.
And the presence of AFib is shown to be very predictive of late mortality with a hazard ratio of 1.48, but I should say, since we've had some excellent talks on sudden death, that AFib does not increase the occurrence of sudden cardiac death, though may lead to inappropriate shocks. And this is a recent paper from [INAUDIBLE] and his colleagues, which showed the survival in patients with AFib to be significantly less. And this is the AFib survival on this bottom line, and the solid line is in patients with no atrial fibrillation.
It's also been shown, and this is a study from the Cleveland Clinic, that if you have post-operative residual atrial fibrillation, that has an extremely negative impact on post-operative survival. And again, you can see this study, which showed a pretty dramatic impact of residual post-operative AFib on freedom from composite events.
And you can see right here compared to no AFib, and I think this is a compelling argument to be very aggressive with AFib, particularly in those patients who are being referred for septal reduction therapy. And certainly that's been my policy. This is a quote from Doctor Barry Marin, where he does say that combining myectomy with the maze procedure has been suggested, although the efficacy of this practice is unknown.
And that's very true. In fact, the largest report I could find in the literature, it was only 10 patients. So I'd like to share with you our experience because, like I've said, my strategy's been very aggressive to pursue surgical ablation. These patients also often are very symptomatic with their atrial fibrillations since the loss of atrial kick is very poorly tolerated. And my preferred strategy has been a biatrial maze procedure.
We developed the maze procedure in surgery for AFib in Saint Louis at Washington University, and we've continued to modify it to make it a much more amenable concomitant surgery. And the one thing in patients with hypertrophic cardiomyopathy, you need to have a well performed, efficient, quick operation. And the advent of simplifying the maze procedure, which we've worked hard on over the last decade, I think has really tremendously improved the results in these patients.
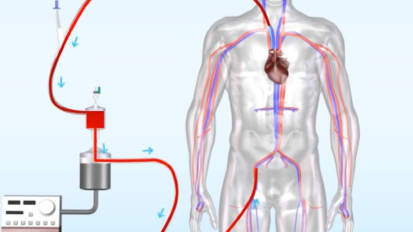
And instead of using surgical incisions, now we use ablation devices, and you can see the lines of ablation in white on patients who have undergone a maze procedure. And this is our present modification when we do it through a sternotomy. And on the left side, we make just one incision and the rest of it's just done with ablation devices shown. And these are the scars that we create in the atrium that have been shown over the last two decades to be very effective in preventing AFib.
We've done 27 consecutive patients with HCM and AFib, and done a combined septal myectomy maze procedure. But these patients have had AFib for about two years. And it's interesting, as opposed to our big population who undergo maze procedures, most of these patients have paroxysmal AFib and are often very, very symptomatic. And you can see the large left atrial size in these patients, which is actually larger than we see in our overall lone AFib population.
96% of the patients are available for follow-up. We had a mean of 4.7-year follow-up. And we didn't see-- it's a small group, but compared to just doing an isolated septal myectomy, we didn't see any increase in the perioperative complication rate of mortality and our late results are excellent. And we compared them to our results with lone AFib shown in yellow. And you can see that the success rate out at two years was 88% freedom from any atrial arrhythmias. And actually, we have results out to five years where over 95% percent of the patients are free of atrial arrhythmias.
So this is a durable, good result in these patients and I think has the potential to both improve quality of life in terms of symptoms and also, I think, will likely lead to a reduction in stroke rate and improvement of survival. And then I'll finally end by just talking briefly about approaches to address residual mitral regurgitation. And that has been quite a hot topic in the surgery community, but one I think that is often overemphasized and particularly in patients from surgeons who aren't that experienced with septal myectomy.
The first thing I'd like to really emphasize is, if you do your septal myectomy correctly, it almost always corrects the systolic anterior motion and mitral regurgitation. And that primary operations to just address the mitral regurgitation are usually not needed and often unduly complicate the procedure. And actually, in large experiences-- and we've talked about the Mayo Clinic and then a recent editorial in JACC. Hartzell Schaff and Rick Nishimura reported that it's very, very unusual, in their experience, to need concomitant mitral surgery and only 2% of all the patients referred to the Mayo Clinic. And that's been our recent experience.
But there are definitely patients that have other organic mitral pathology unrelated to the Hokum physiology, and in those patients mitral repair is indicated and does require careful attention and planning. And it's actually quite different, the approach of those patients, particularly if they have degenerative MR, than when you see patients who have that without hypertrophic cardiomyopathy.
And in those patients, we do favor anterior leaflet patching and an Alfieri stitch to prevent any systolic anterior motion. And that's just due to the fact that has been stated before, and you saw on that beautiful echo that Doctor Bach showed, that you get systolic anterior motion of this anterior leaflet and that it plays a role in the outflow tract obstruction.
Unfortunately, with our standard technique of mitral repair, which is to put a ring in, we tend to push that anterior leaflet somewhat back into the outflow tract. And in a normal patient that's not a problem, but in a patient with hypertrophic cardiomyopathy, that can result in worsening that obstruction and complicating their post-operative course.
So there's some techniques that we have developed-- that have been developed-- that prevent that systolic anterior motion. And I think one of the first techniques, that was first described from the group in Rotterdam, was to patch the anterior leaflet. We've modified that somewhat, and they described patching it through the aortotomy. And you can see this is the similar view, and you can see the myectomy here and this is the patch they put.
This is actually quite cumbersome and I think would only be indicated in the patient with a really excessively long anterior leaflet. That would be a different type of pathology, but in a patient with just purely degenerative MR, we favor patching it through the left atrium than patching the anterior leaflet in this way, which really does stiffen the leaflet and prevent the SAM.
Another easy technique that has been described for mitral repair is just a simple stitch in the middle. Stitching the anterior and posterior leaflet together. It actually has been shown in big studies not to result in any mitral stenosis when done in the correct patients, and particularly these patients who usually have big mitral annulus. And that also is a nice technique.
And these are techniques that really have made the need to ever replace the valve really not-- there really is no need to ever replace the mitral valve. So I think these are, I think, nice little strategies for surgeons to have to prevent that. Another very recent report that was just recently published in JACC described transaortic chordal cutting, also to help prevent the systolic anterior motion and particularly felt to be helpful in patients who have mild septal hypertrophy.
And this is an interesting technique, and not one that I personally have much experience with, but seems to make some sense where you could do-- through the aortic valve-- cut the secondary chords of the anterior leaflet, relieving the obstruction. And I think that, certainly in this small series, had some excellent results. And here you can see the preoperative resting outflow tract gradient and the post-operative gradient you can see really superb results again from the group in Italy.
In conclusion, I'd like to say I think surgical septal myectomy is really the gold standard for the interventional treatment of hypertrophic obstructive cardiomyopathy and really has excellent late symptomatic improvement and improvement in gradients. And I think that there are definitely now minimally invasive approaches, which I think certainly make the operation maybe a little more palatable to most patients and I think will end up limiting even further the morbidity of these procedures.
And I think it's important to remember surgical septal myectomy offers the advantage of being able to address other cardiac anomalies, and particularly atrial fibrillation, which I think is not addressed often enough in this population associated with mitral pathology, coronary disease, and as Richard said, with not infrequent occurrence to see patients with other outflow tract abnormalities. Thank you very much. It's been a pleasure.
Minimally invasive septal myectomy procedures, atrial fibrillation is an under-recognized problem in HOCM patients.
Visit the following links for more videos from the 2015 AHA Symposium:
Part 2: Preventing Sudden Cardiac Death in HCM
Part 3: Cardiovascular Magnetic Resonance in Hypertrophic Cardiomyopathy
Part 5: What Clinicians Need to Know About Genetic Testing for Patients and Families with HCM
Related Presenters
Evarts A. Graham Professor of Surgery, Chief of Cardiothoracic Surgery, Co-Chair, Heart and Vascular Center Barnes-Jewish Hospital
Related Videos