The morning of February 7, 2014 was supposed to be an uneventful one for Arlene Whitmore, a 62-year-old kindergarten teaching assistant in Anne Arundel County, Maryland. But when she swung her legs out of bed, she immediately noticed something strange: her right leg heavy and numb, like it was asleep. The feeling persisted over the next several days.
“I thought I must have pinched a nerve,” Whitmore remembers.
But the problem was much more serious. Over the next several months, she bounced from provider to provider, including her family physician, chiropractor and a local neurologist. Her providers ran numerous exams, including blood tests for Lyme disease and markers of multiple sclerosis, and imaging tests including multiple MRIs. None turned up anything suspicious.
All the while, the function in her right leg, and then her left, gradually declined. She transitioned from a walker to a rollator to a wheelchair, eventually becoming bedridden. Edema creeped into both affected limbs, ballooning them both into extreme proportions. In the meantime, she says, no one could figure out why any of it was happening.
She finally had a breakthrough nearly a year and a half later after a friend suggested she see Johns Hopkins neurologist Justin McArthur, director of the hospital’s Department of Neurology. After a thorough review of Whitmore’s substantial medical records, McArthur says he had a strong suspicion of what might have caused her paralyzing cascade.
— Justin McArthur
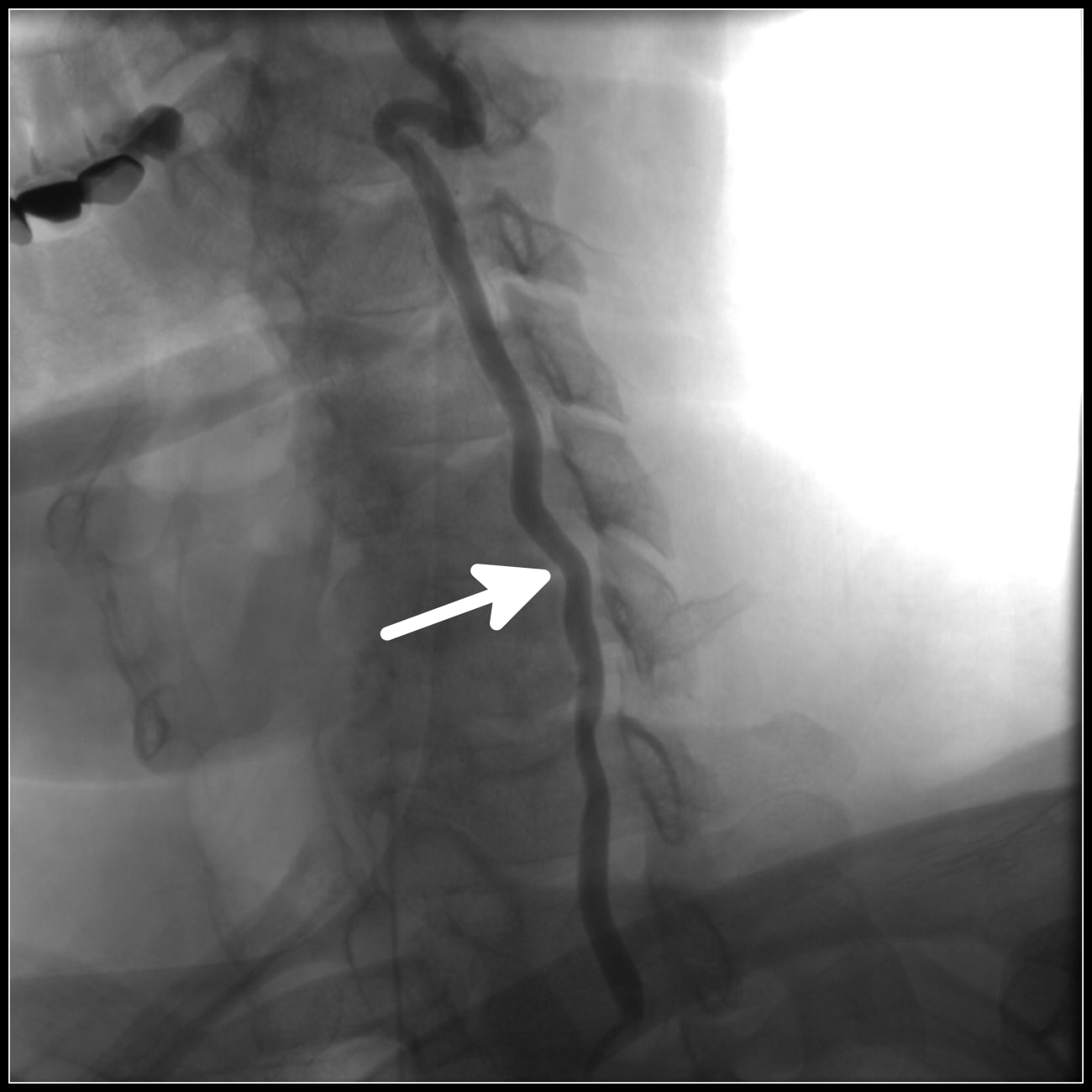
He referred her to the Johns Hopkins Transverse Myelitis Center, a hub for experts in the disease of transverse myelitis itself, but also for a variety of other conditions that affect the spinal cord. Under the guidance of McArthur’s colleagues Carlos Pardo-Villamizar and Phillipe Gailloud, Whitmore underwent a spinal angiogram, showing concretely that she’d undergone a spinal cord stroke — a rare manifestation of neurologic ischemia. The extreme infrequency of this condition, affecting only a few patients in the U.S. per year, and Whitmore’s unconventional presentation of gradual decline stymied her timely diagnosis, McArthur explains.
But now that they had an answer, McArthur and Whitmore worked together to create a plan to improve her function and stave off further complications. With his support, she’s been involved in an intensive physical therapy protocol for the past three years under the guidance of a therapist who has experience with spinal cord stroke patients. She’s made slow but steady progress, gradually relearning to walk over time. Now, she has significantly more mobility, walking with the assistance of a cane.
“We want to send the message to patients to never give up. There is always something that can be done, whether it’s rehabilitation or symptomatic treatments,” McArthur says. “With multidisciplinary care and Arlene’s incredible motivation, she has overcome tremendous odds.”