A Q&A with Johns Hopkins psychiatrists Angela Guarda and Colleen Schreyer
Interview and text by Benedicta Kim and Karen Blum
For decades, experts with the Johns Hopkins Eating Disorders Program have challenged the nutritional prescriptions of traditional treatment programs for eating disorders “to start low and go slow.” This has decreased the time needed to restore weight, normalize eating and weight control behaviors, and master relapse prevention skills needed for successful long-term recovery from anorexia nervosa. The Johns Hopkins team has helped hundreds of patients resume schooling, work and relationships interrupted by illness.
Angela Guarda, director of the program and the Stephen and Jean Robinson Professor of Eating Disorders, has called for universal reporting of clinical outcomes by eating disorders treatment programs to increase transparency and help patients, families, providers and payors compare treatment approaches. Headed by Colleen Schreyer, director of clinical research for Johns Hopkins’ longitudinal eating disorders outcome project, the clinical research team has focused on assessing and publishing the program’s treatment outcomes in a series of peer-reviewed articles published in the International Journal of Eating Disorders. The research team’s work reports on treatment outcome variables, including the average rate of weight gain, percent of patients who achieved a minimally healthy weight, safety of the meal-based rapid nutritional rehabilitation prescription, relative cost of treatment, and relapse risk. They also examined patients’ perceptions of treatment, and whether patients felt they benefitted from the program’s rapid weight gain, meal-based, behavioral approach.
In this Q&A, Drs. Guarda and Schreyer explain the rationale for the program’s approach to treating anorexia nervosa and discuss its treatment outcomes and research findings.
Dr. Guarda, before we delve into The Johns Hopkins Eating Disorders Program’s outcomes research findings, could you provide us some background on how patients feel when facing treatment? What is the “anorexic mindset”?
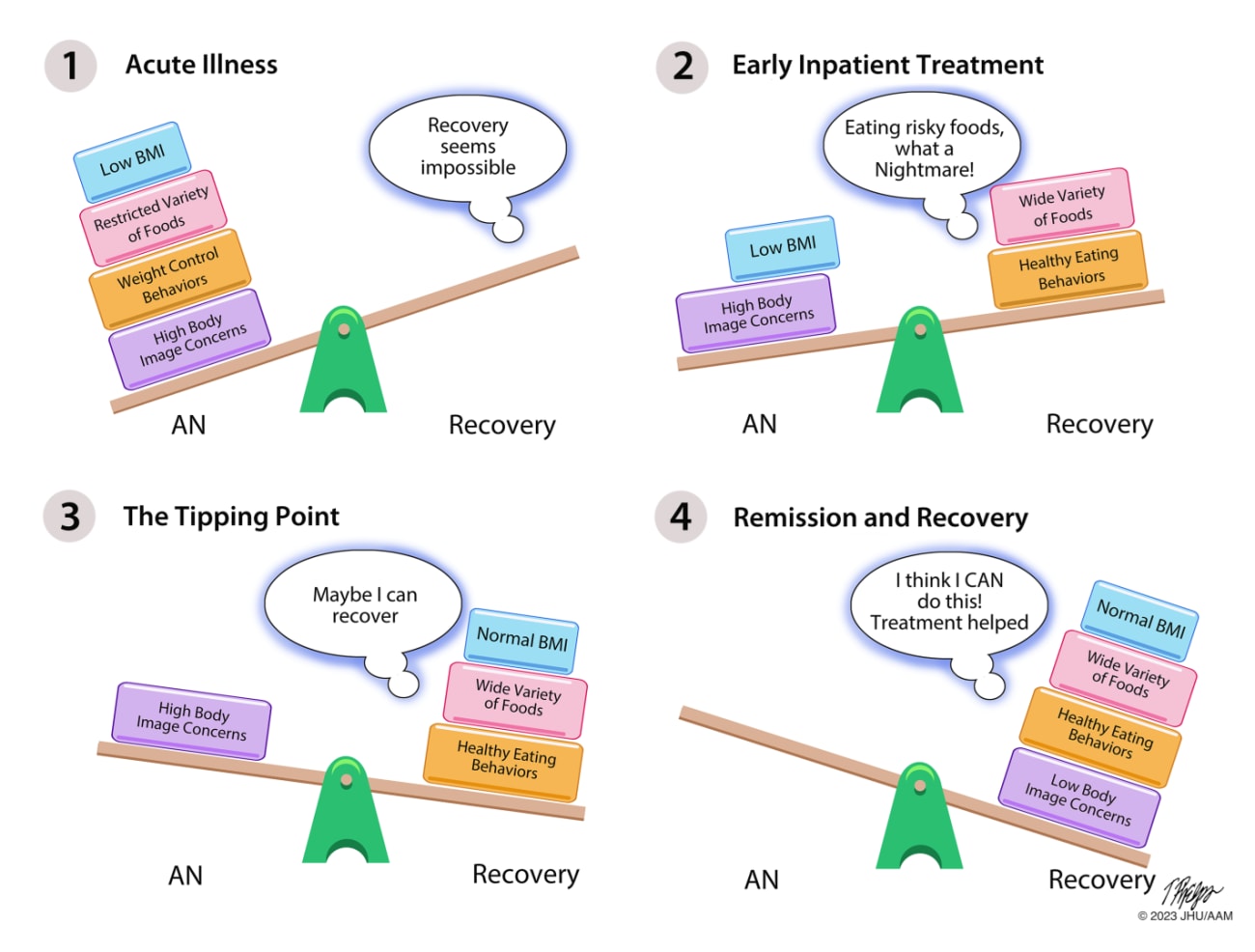
Anorexia nervosa increases anxiety about gaining weight and eating high-calorie foods — and yet this is necessary for thoughts, mood, and body dissatisfaction to improve in patients with the disorder. Key goals of treatment are weight restoration and eating a variety of foods of differing calorie densities at regular meals. We know the starved state and a restricted food repertoire perpetuate eating disorder thoughts and feelings, and alter brain function, so achieving these goals are crucial first steps in recovery — but ones that often feel overwhelming for patients. The Johns Hopkins Program helps patients overcome anxiety about eating and employs a behavioral, meal-based, rapid-weight restoration approach to (1) minimize time spent in intensive treatment; (2) help patients normalize their eating and weight control behaviors and overcome anxiety about eating; and (3) master skills needed to prevent relapse once back at home. The approach is team-based, collaborative, and it includes group, family, nutritional, and occupational therapies.
Dr. Guarda, could we say weight restoration and being able to eat a variety of foods is central to having a “non-eating disordered or healthy mindset”?
In a sense, yes—anorexia nervosa hijacks the healthy brain. Our brains consume 20% of our daily caloric needs; a starved brain simply does not think clearly – and talk therapy is less effective when someone is in a starved state. Furthermore, searching for explanations or a “root cause” — as to why a person developed anorexia — is not enough to get someone well. It’s not so much an “aha moment” of insight that leads to change: We need to help patients change their behavior and restore nutritional health for anorectic thoughts and feelings to gradually fade. That’s what makes weight restoration and normalized eating crucial treatment priorities. In the absence of headway with those, no amount of therapy alone is likely to help someone get well.
Dr. Guarda, the Johns Hopkins program’s average weight restoration rate is four pounds a week — double that of most programs. Is it safe?
Yes, back in 2015, we published a study that included 461 consecutive underweight patients and found that the program’s meal-based, rapid weight-gain behavioral approach coupled with close medical monitoring was safe and effective and did not result in higher risk of a dangerous complication known as refeeding syndrome. Additionally, over 70% of patients left treatment weight restored and at a healthy weight, following a shorter admission and without the need for nasogastric tube feeding. At the time, this approach went against the general belief that restoring weight at a rate greater than 2–3 lbs per week was dangerous and could lead to serious risk. Indeed, partly as a result of this study, the recently updated American Psychiatric Association’s Practice Guidelines for the Treatment of Eating Disorders now recommends that residential and inpatient programs should achieve average rates of weight gain of 2–4 lbs per week for anorexia nervosa. Thanks to a faster rate of weight restoration, most patients reach a minimally healthy weight over weeks rather than months. Faster weight gain means less time away from home, work, or school and, in the long run, less costly care.
Dr. Schreyer, in the longitudinal study — when you followed up with patients after hospitalization — what were the key predictors of good outcomes?
Consistent with the importance of restoring weight, we found that weight at program discharge was more important to avoiding relapse six months later than was age, number of past hospitalizations, or how long a patient had been ill with anorexia. Additionally, patients who reported higher confidence in their ability to eat in a healthy balanced pattern at hospital discharge were less likely to have relapsed six months later. And, despite the rapid weight gain and behavioral focus of the program, patients reported being highly satisfied with the treatment they received. About 83% said they would recommend the program to others. As one patient put it: “With anorexia, any rate of weight gain feels too fast — I’ve lost enough time already because of this illness.”
Dr. Guarda, 83% patient satisfaction with this approach is impressive, given that patients are anxious about weight gain. How is this possible?
Focusing on rapid nutritional rehabilitation and normalizing eating and weight control behaviors may feel anxiety-provoking at first, but when addressed in the context of a specialized behavioral treatment program that incorporates close medical management, family support, group therapies and a collaborative team-based approach to care, patients support one another, learn to lean into their anxiety, disengage from eating-disordered thinking, and achieve mastery over the disorder. In a sense, recovery from anorexia requires unlocking the healthy brain through nutrition, behavior change and psychotherapy — and mastering the tools and skills needed to maintain healthy function and avoid relapse.
Dr. Schreyer, how did the pandemic affect patients in the program?
The COVID pandemic has taken a toll on everyone especially on adolescents — we are seeing a worldwide increase in eating disorders in youth. At Johns Hopkins, we found that adolescents admitted to the program from March 2020 to March 2022 were arriving with more severe eating disorder, depression and anxiety symptoms. Despite this heightened clinical severity, outcomes including weight regain were similar to those of patients admitted before the start of the pandemic. That means we were equally effective in treating these patients, even though they presented as more severely ill.
Dr. Schreyer, we’ve been focusing on anorexia, could you walk us through avoidant/restrictive food intake disorder (ARFID)?
Avoidant/restrictive food intake disorder, or ARFID, is a recently defined eating disorder in which patients restrict their intake due to low interest in food, sensitivity to food odors, tastes or textures, or fear of consequences of eating (e.g., choking, vomiting, or stomach pain). Importantly, patients with ARFID do not endorse marked body image concerns, however their restricted food intake results in a malnourished state and impaired function. The Johns Hopkins weight restoration protocol is effective in treating underweight patients with ARFID. Although weight gain rates were slightly lower for patients with ARFID compared to those with anorexia nervosa, a similar majority of those with ARFID clinically improved and achieved a minimally healthy weight by discharge.