Pediatric Heart News
December 13, 2013
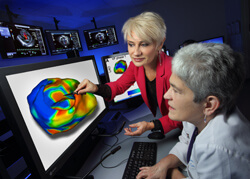
“Pediatric cardiologists have long sought a way to optimize device placement in this group of cardiac patients,” says Johns Hopkins biomedical engineerNatalia Trayanova, “and we believe that our model is a critical first step toward bringing computational analysis to the pediatric cardiology clinic.”
To build the model, the team began with low-resolution MRI heart scans of a child born with tricuspid valve atresia who’d had a modified Blalock–Taussig shunt, bilateral bidirectional Glenn shunts and a Fontan procedure using an extracardiac conduit. Based on these images, investigators developed a 3-D computer model that allowed them to simulate ventricular fibrillation and then predict how effectively the defibrillator would terminate the arrhythmia when located in each one of 11 positions around the heart. The model revealed that two particular positions rendered therapy optimal.
A particular advantage of the model is that the team used digital representations of the heart’s subcellular, cellular, muscular and connective structures—from ions and cardiac proteins to muscle fiber and tissue—and also included the bones, fat and lungs that surround the heart.
“Heart function is astounding in its complexity and person-to-person variability,” Trayanova says, “and subtle shifts in how one protein interacts with another may have profound consequences on pumping and electric function. We wanted to capture that level of specificity to ensure predictive accuracy.”
Less-than-precisely positioned defibrillators can fire unnecessarily or, worse, fail to fire when needed to shock a child’s heart back into normal rhythm. In addition, devices that are not positioned well can deliver ultra-strong, painful jolts that can damage heart cells and increase risk of death.
“These are lifesaving devices,” says Johns Hopkins pediatric cardiologist and arrhythmia specialistJane Crosson, a member of the study team. “But they can feel like a horse kick to the chest and really traumatize children.”
In their study, the researchers considered the best configuration to be the placement that exhibited the lowest defibrillation and cardioversion thresholds. If further studies show the model has value in patients, it could spare many children with heart disease from repeat procedures that are sometimes needed to reposition the device.
