Chapters
Transcript
TUN JIE: This is a patient that had history of adrenal cancer. Had the surgery many years ago. Developed a colon cancer and had a little bit of mass.
Patient underwent a new adjuvant therapy, had a colon resection. And now is coming back to me for liver resection. On the pre-staging imaging, there was one lesion at the segment five behind the gallbladder.
We attempted to do this laparoscopic, but due to previous surgery, two dense adhesions as you can see. We can't even see the liver. So what I'm going to do is do a take down adhesion. I'm going to use a THUNDERBEAT to take down this omentum adhesions right here.
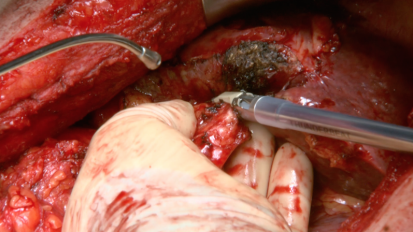
So interop, we encounter a lot of this granuloma. The question is so, if I brought in material from previous surgery or something else. I doubt this is a cancer recurrence, which is unusual because he had a colon surgery recently. I think it's just granuloma from the previous surgery. But nonetheless, we're going to resect this and send the pathology for examination.
Try not to go too low. Yeah, that's fine.
So I use a coapp button to achieve a-- so see you see the liver is right here.
All right. So this is the stomach. Unfortunately these are structures of very well vascularized. Any tissue from the stomach-- basically you're talking about a great omentum.
So you can easily do an enterotomy if you're not careful.
The good thing is when the stuffer off the perineum, you only worry about the bleeding from one side. It's not going to bleed from the perineum side, right? Because the rest was not coming from there.
Some people use this as a retraction, and I don't.
The clip.
So wrong ligament.
So that's sent to the pathology. So far I immobilized the left lobe. And the next step, I'm going to immobilize the right lobe. And then hopefully we can-- OK, turn the table towards me now.
SPEAKER 2: Looks like you're making a [INAUDIBLE] adhesion.
TUN JIE: I know. Console please.
I mean, that's the whole problem. He has so much of-- somebody done before. So I see the gallbladder now, finally.
I was thinking well, that's my first step, do a laparoscopical cystectomy. Wrong. We have so much of adhesion.
So basically I want to see one lesion. Suspicious, which is corresponding to the finding on the MRI. So I already marked the surgeon margins. So we're going to do a resection.
The lesion is centered right here. So what we're going to do is first we develop a tissue print on the side. One second.
That's OK.
My first tissue print is going to be right here.
So [INAUDIBLE]-- so the way that-- nope, give it to me.
Pretty good homeostasis so far.
So I usually don't take a big bite. Just take a small bite.
Ultrasound. Have to use ultrasound to look here.
So wow, this is pretty close. I don't like. You see this side? Too close. So we may have to go a little bit bigger.
The lateral side, you see that? In the margin right there. But the superior side is fine.
So basically I want to create a border around the resection of the tumor and then slowly going in-- obviously the geometry distribution of the tumor doesn't conform to what the natural approach of this is. So basically I try to develop a notch in superior. And hopefully then inferiorly. And eventually I can get the resection accomplished.
So the lesion itself actually is quite challenging because of location. It's right at the segment five. And I'm not far away from some of the major vessels.
So what I'm doing is try to approaching it from a good margin.
Typically I want to want to have a one centimeter margin if possible. I want to divert the lateral margin, which is right here.
So I'm working on the lateral border one more time.
Get the scalpel. I'm going to cut this piece out.
Almost tempting to just-- it's geometrically much easier to approach it.
SPEAKER 3: You can do it.
TUN JIE: But then typically, the philosophy is do parenchyma-sparing. You don't want to cut as much as you want. Well, you cut as much as you need, not as much as you want.
Obviously right lobe resection is much better. That's probably not very good for him.
I think the inferior, I cannot interrupt the inferior.
OK. Go by four, now let's go back there. Got it.
So what I'm going to do is just type inferior and start [INAUDIBLE] from above because we have a good-- I think we have good [INAUDIBLE] right here.
So I'm going to start around tangential [INAUDIBLE] resecting.
Suction. OK good, excellent.
Watch out. Ultrasound?
I see a vein right there. Suction. Give me a--
SPEAKER 3: [INAUDIBLE]
TUN JIE: No.
SPEAKER 4: That would be a main [INAUDIBLE] pathology? I just want to be clear. You can call the pathology and just let them know that I'm coming out in about two minutes.
SPEAKER 4: OK, and what should I call it?
TUN JIE: Segment five lesion. We want that margin.
SPEAKER 4: Seven five--
TUN JIE: Segment.
SPEAKER 4: Segment five lesion.
TUN JIE: I want the surgical margin. I'm going to bring the specimen to pathology.
I see the vein right here. You probably see a little bit too.
SPEAKER 3: How much longer are [INAUDIBLE] main branch?
TUN JIE: Medial. But you're right, you can't tell. But then the thick of your vessel usually can give you some hints. The portal vein usually had the portal triad structure around it. And therefore--
SPEAKER 4: [INAUDIBLE] forgot to call. And he says he'll be down here in about 15 minutes.
SPEAKER 3: OK, thank you.
TUN JIE: Can you have the patient's head down please?
SPEAKER 3: Head down.
TUN JIE: That's good.
SPEAKER 3: The meter is over now so I guess once the [INAUDIBLE] is out.
TUN JIE: Yeah, that's fine.
Yes, you see that fibrotic material.
SPEAKER 3: Right here?
TUN JIE: Yeah. See there's a clip right there in this way.
Suction.
So basically this patient had a history of adrenal cancer. Had surgery done many years ago. Developed colon cancer, and recently had underwent a new adjuvant therapy. Had the laparoscopic colon resection. And he was found to have a solitary lesion at segment five right around the gallbladder proper.
He also had a history of a portal vein thrombosis. So what we have performed is an attempt to do this laparoscopically. Unfortunately he had so much of a lesion we had to convert the procedure to open.
We explored the whole liver. We performed the [INAUDIBLE] ultrasound. As we expected, there was a solitary lesion at the segment five. So we perform a wedge resection.
Well I think as you can see, the homeostasis is pretty good. I mean obviously in the past I have used a different instrument like staples or cauteries. The problem with the staple is often times because of the configuration of the liver, it's hard to perform a limited parenchyma-sparing resection, often times resulting in a resecting bigger parenchyma to accomplish the satisfactory margin.
I think this divisor provides us some ability to do a parenchyma-sparing resection with achieve a satisfactory outcome.
University of Arizona Interim Chief and Assistant Professor of Surgery, Dr. Tun Jie, performs a Segment V Liver Resection with THUNDERBEAT.
Related Videos